
Close

Subscribe to out newsletter today to receive latest news administrate cost effective for tactical data.
96 Clinton Ave, Newark, NJ 07114, United States

Boost your revenue with Medexa RCM’s advanced billing solutions. Our RPA-powered system ensures 99% claim accuracy, 26-day payments, free credentialing, 20% revenue growth, and steady cash flow through proactive A/R follow-ups.
500+ Physicians
40+ Specialties
Medical Billers & Coders
RPA Billing Solutions
Clean Claim Rate
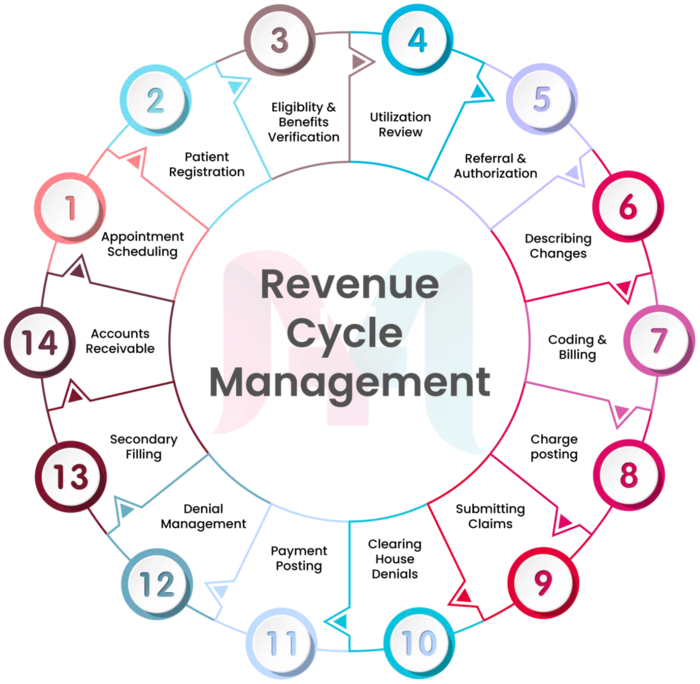
At Medexa RCM, we take a comprehensive, technology-driven approach to Revenue Cycle Management (RCM), optimizing every step of the patient-to-payment process. We begin with accurate patient registration and eligibility verification to capture precise information and minimize claim denials. Our certified coding specialists handle ICD-10 and CPT coding with care, ensuring proper charge capture, maximum reimbursement, and reduced compliance risk. By leveraging advanced RCM technology, we monitor claims in real time, proactively identifying and resolving issues to keep your revenue cycle running smoothly. Our team also manages denial prevention, appeals, and revenue recovery, helping you secure payments that might otherwise be lost. We provide timely payment posting and financial reconciliation, giving your practice complete visibility and control over its cash flow. With Medexa RCM, healthcare providers experience faster reimbursements, fewer administrative burdens, and a streamlined financial process that strengthens both revenue and patient care.


Support Line 24/7
Online Schedule
Achieve an impressive 99.9% uptime to ensure continuous RCM services availability.
Rigorous measures are in place to meet and exceed HIPAA regulations.
Adhered to both SOC-1 and SOC-2 protocols for the highest industry standards in security.
We ensure data accessibility through robust disaster recovery measures.
Medexa RCM delivers tailored billing solutions for primary care, specialty clinics, and surgical centers — ensuring accuracy, faster reimbursements, and HIPAA compliance.













Our RCM services begin with efficient appointment scheduling. By leveraging advanced scheduling systems, we optimize appointment slots, reducing wait times and enhancing patient satisfaction. .
Read More
Accurate and detailed patient information is the foundation of effective medical billing. Our patient registration process is meticulous, ensuring that all necessary details are captured..
Read More
Our front desk management team ensures that patients’ eligibility and benefits are verified accurately before services are rendered..
Read More
Our utilization review ensures that the medical services provided align with HIPAA guidelines, optimizing reimbursement while maintaining insurance compliance..
Read More
Our RCM services navigate the complex landscape of referral authorization. We ensure that necessary approvals are obtained and prevent claim denials and delays..
Read More
We ensure that any changes in coding, billing, or regulatory requirements are promptly implemented, reducing the risk of compliance issues..
Read More
Our team of experienced medical billing specialists employs accurate coding practices, eliminating cash flow inconsistencies..
Read More
We ensure that charges are posted on time, contributing to a robust cash flow framework. .
Read More
By adhering to practice standards and using advanced technology, we expedite the claims submission process. .
Read More
Our experts promptly address claim denials, identifying root causes and implementing corrective measures to prevent future issues. .
Read More
Our systems ensure that payments are posted promptly directly to the provider’s account. .
Read More
Our billing specialists give effective denial management strategies involving a systematic approach to identifying and preventing claim denials. .
Read More
For claims that require secondary filing, we ensure a seamless process, maximizing reimbursement opportunities and reducing the risk of revenue loss. .
Read More
Our AR specialists handle the posting of payments received from insurance companies and patients to improve turnaround times. .
Read More
Our appeal procedure is well-defined, addressing denied claims through a strategic appeals process. .
Read More
Transparent and accurate patient billing is a priority for Transcure, fostering positive patient experiences. .
Read MoreMedical billing is the process of submitting and following up on claims to health insurance companies to get paid for medical services. This process is complex and involves several steps, starting with patient registration, demographic entry, and insurance verification. Once those steps are complete, the process moves on to charge entry where services are added, then medical coding, where medical procedures are translated into CPT and ICD-10 codes. Then claim submission where the coded claims are sent to insurance for payment.
Our fee is a transparent starts from 2.99 % of net collections—no hidden charges.
We import your payer rules, set up ERA/EFT, and go live in 14 days.
Revenue cycle management (RCM) is the total process of managing the finance of a healthcare organization from patient registration to payment posting. This complex process has many steps, including managed billing, charge capture, coding and insurance verification. Effective RCM allows healthcare facility providers to have an improved cash flow, reduce administrative burdens and optimize their finances. By managing the entire revenue cycle, healthcare specialists can focus more on patient care while keeping their financial house in order.
Medical billing is the process of submitting and following up on claims to insurance companies to get paid for services rendered by healthcare providers. It’s a big part of the revenue cycle and directly affects the financial health of medical provider.
We handle claim denials by thoroughly analyzing the root cause, correcting errors, and promptly resubmitting the claims. For appeals, we gather necessary documentation, follow payer guidelines, and advocate for accurate reimbursement.
Yes, absolutely! We utilize real-time claim scrubbing software to identify and rectify errors before submission. By addressing incomplete information, coding errors, and insurance verification processes, we can streamline billing and improve efficiency.